6 Surprising, Common Causes Of Pelvic Pain You Should Know
“Your estrogen levels plummet within the first 48 hours after giving birth,” says Sherry Ross, MD, OB/GYN, women’s health expert and author of She-ology: The Definitive Guide to Women's Intimate Health. Period. At the same time, your body increases production of the hormone prolactin to stimulate milk production for breastfeeding. Why is this hormonal shift a problem? Estrogen helps keep the vagina naturally lubricated, so when levels are low, it can cause vaginal dryness and low libido. And, the dryness can lead to pelvic pain during sex. "The friction in the vagina caused by the penis can be intolerable if there isn't the vagina's normal mechanism to get wet with sex," Ross says. “Treatment usually involves time, patience, and a little K-Y jelly." (Buy K-Y Jelly for $6.79 on amazon.com.)
Even if you're not a new mother, you might notice pain in the pelvis area when having sex. "Pelvic pain is often felt deeper and inside the abdomen," Ross says, and this could happen from tears or lacerations, as well as irritation to the cervix, which can happen from rough sex. Don't confuse this kind of pain with pain from vaginal dryness, she says: "Vaginal dryness tends to cause pain only in the vagina and is not experienced inside the lower abdomen." If you have irritated your cervix or uterus, you will want to see a doctor to discuss next steps and ways to minimize the pain.
Certain sexual positions are also known to be anatomically harder on the vagina and female organs, including the uterus and ovaries. The “Missionary” position tends to be easier for women and their anatomy, whereas “Doggie Style” (from behind) allows for deeper penetration for the male but more discomfort and pain for many women, she says. “It’s completely normal for women to experience pain during sex depending on certain sexual positions. Learn and know what positions are less uncomfortable and painful during sexual intercourse with your partner." (And, FYI, these are the best sex positions for every age.)
If you suddenly notice pelvic pain, it could be related to an STI, says Ross. “Sexually transmitted infections such as chlamydia and gonorrhea are the typical culprits of serious pelvic infection that can lead to pelvic pain and infertility,” she says. These STIs can result in pelvic inflammatory disorder (PID), she says, which can trigger fever, chills, abdominal pain, vaginal discharge, nausea, and vomiting. While it can be treated with oral or IV antibiotics, make regular appointments with your gynecologist to detect infections early. “Getting STI checkups between new sexual partners is so important to ensure you are not a carrier of damaging STIs,” Ross says.
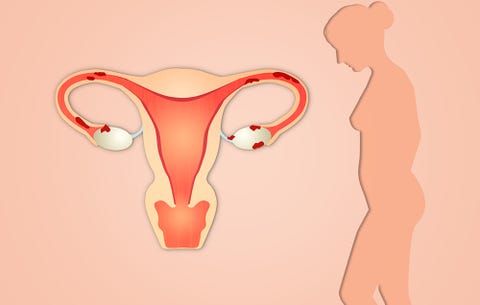
Here's another reason for pelvic discomfort that can make your monthly flow feel even more brutal than normal. Endometriosis is a condition where the uterine lining starts to grow outside the uterus, and it can cause stabbing pain, as well as gastrointestinal issues, painful breathing, upper body aches, and frequent urination. However, these symptoms overlap with other conditions, so you'll want to get diagnosed for endometriosis to make the distinction and treat your pain properly.
Ladies, it happens—but you don’t need to suffer through pain down there while going through "the change." Because your estrogen levels drop during menopause, “vaginal dryness can also occur in menopausal women who are not taking any estrogen, which results in a burning sensation inside the vagina, especially with sex,” Ross says. “Sexual lubricants, estrogen cream, and Osphena, a non-estrogen oral therapy, can help with some of these problems related to dryness." A newer, non-medication option is MonaLisa Touch, a laser therapy for vaginal atrophy—here's how it works.
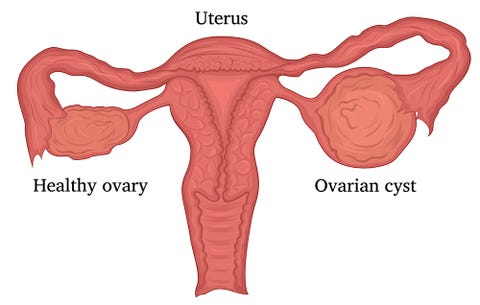
If you are ovulating, or “mid-cycle," chances are there's a large ovarian cyst waiting to burst and release the egg, Ross says. “Aggressive sex, exercise, or a spontaneous rupture can cause this cyst to release its fluid contents along with the egg, causing noticeable pain,” she explains. A pelvic ultrasound and your menstrual history can help your doctor diagnose your pain.
Latest Posts
- Vaginal Odor: What’s Normal and What’s Not
- How Your Vagina & Vulva Change in Your 30s, 40s & Beyond
- The Clitoris Is Important for This Reason, Too
- 5 Ways You Change Down There As You Get Older
- Does your vagina actually age? Here are 6 things that happen to your vagina as you get older